Stroke and Carotid Disease
What is a stroke and what are my carotid arteries?
A stroke is when there is a compromise, or an interruption, to the blood supply of the brain. The brain tissue is extremely sensitive to any small change in blood supply. One of the more common strokes is when the arteries supplying the brain become blocked. This leads to what’s called an ‘Ischemic Stroke’. Ischemia implies a lack of oxygenated blood. The carotid arteries supply the brain with blood from the heart along with the two vertebral arteries.
There are many other forms of stroke, such as a hemorrhagic stroke (which means a bleed in the brain which causes a reduction in normal oxygenation of brain tissue), an embolic stroke (which is a result of small and in some cases microscopic matter or debris lodging into very fine small blood vessels in the brain) and even complete ischemic stroke from a completely blocked carotid artery.
What do carotid arteries do?
The carotid arteries exist in the neck region on both left and right (the normal anatomy is to have two carotid arteries). These are major branches off the aorta. The aorta that arises directly off the heart.
The carotid arteries on both left and right divide in the neck into an external and internal carotid artery. It’s the internal carotid artery that then travels into the base of the skull to supply your brain with fresh and plenty of oxygenated blood directly from the heart. The external carotid artery supplies the face and the sinuses.
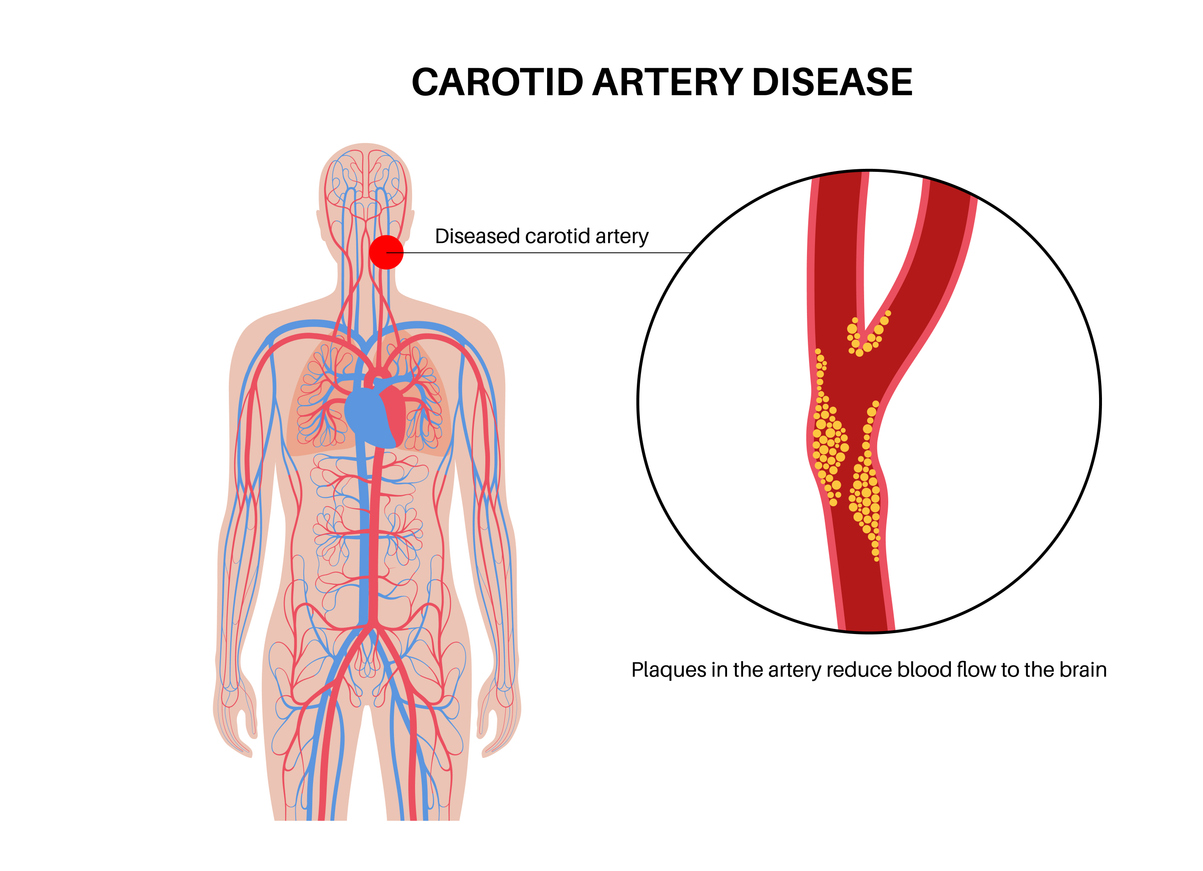
At the bifurcation of the Common carotid artery (into the internal and external carotid arteries) there is a common location for where plaque can build up.
What is stenosis of the carotid arteries?
The Common Carotid Artery (CCA) bifurcation, is where there is a structure called the carotid sinus, which is a bulb-like structure extending into the origin of the Internal Carotid Artery. It is this area that, due to factors that are not entirely understood, becomes susceptible to plaque build up.
As the Plaque builds up it starts to encroach and invade the space in the middle of the artery (the lumen of the artery). As it does this the blood struggles to safely travel through the artery in order to reach its final destination, in this case for the internal carotid artery that destination is the brain.
What is Plaque?
Plaque is a process of inflammation in response to injury to the internal wall of the artery. It has long been understood that once the injury to the internal wall of the carotid artery starts, then this process sets off a cascade of factors that eventually builds into plaque.
One of the most common causes of injury to the internal wall was smoking. Other causes include high blood pressure and also to some extent high cholesterol (although high cholesterol is more likely related to the acceleration of plaque and not necessarily the initiation).
Plaque has been studied for decades and the content has been very variable but we know that it is rich in cholesterol along with other molecules. It is for this reason that cholesterol management plays a big part in vascular management.
As plaque builds up it forms a stenosis of the arteries. With every heartbeat of blood and flow through the stenosis, any fragility or plaque rupture can result in small plaque debris getting thrown into the brain and causing an embolic stroke.
Does carotid artery stenosis cause stroke?
Once carotid artery stenosis develops the risk of stroke increases. The way in which stroke could occur is through the plaque itself rupturing or breaking off into the blood flow to the brain itself (embolic) or it could rupture and occlude the entire vessel and cause a major ischemic stroke.
This risk is what we as clinicians and vascular surgeons in particular spend our careers focussed on trying to minimise. There is a large body of evidence and well regarded literature that scrutinises the level of risk associated with carotid artery stenosis and the need for intervention.
The question that is constantly facing us and the patient is, does an operation, or a procedure, help reduce the risk of a carotid artery stenosis? And if so, is that risk reduction greater than just using medication alone? The reason why this question is so important is because the procedure itself carries a risk of stroke, and therefore we as surgeons and interventionalists need to be sure that we are only helping the patient and not causing more harm.
Such decisions are not taken lightly and informed consent of a patient comes down to an understanding of the risks and benefits in addition to rapport and trust that is developed between the surgeon and the patient.
What is the management of carotid artery stenosis?
Carotid artery stenosis is managed with two main strategies. The first strategy is making sure that the patient is on the best possible medications that can firstly reduce the risk of stroke, and secondly stabilize or slow the progression of the stenosis (the plaque). The second strategy is intervention.
Intervention for carotid artery stenosis involves removing or reducing the stenosis by either surgically taking out the plaque (carotid endarterectomy) or opening up the stenosis with a stent (carotid artery stenting).
What is the best medical therapy for my carotid artery stenosis?
Best Medical Therapy involves oral medications that act to reduce the risk of clot forming through the stenosis (with the help of an oral antiplatelet drug such as aspirin or clopidogrel) and stabilising the plaque (with the help of cholesterol lowering medications such as Atorvastatin, Simvastatin, Rosuvastatin or Ezetimibe).
In addition to these oral medications, risk factor modification is essential and involves eliminating any smoking or smoking exposure, blood pressure control and also blood sugar control.
What is a Carotid Artery Endarterectomy?
A carotid artery endarterectomy is when the plaque causing the narrowing or stenosis in the internal carotid artery is surgically removed, leaving behind a widely open and clean artery to carry on supplying the brain with oxygenated blood without the risk of throwing off (embolising) cholesterol heavy plaque.
This operation can be performed under a general anesthetic and also under heavy numbing medication in the neck and the patient kept awake. There is a benefit to having this surgery awake in that it may guide best management and allows your surgeon to monitor your brain function throughout. There is no pain felt during the procedure and you are kept lightly sedated.
The surgery involves an incision through the neck and clamping of the artery above the plaque and below. The artery is then opened and the plaque removed. The artery is then closed with a patch which prevents the artery from becoming narrowed and scarred up.
Recovery is only usually a few days and you may be even discharged a couple days after the surgery.
What is a Carotid Artery Stent?
A carotid artery stent often involves a small minimally invasive puncture or entry through the groin artery (femoral artery) and with the help of X-ray vision a stent is deployed over a wire in the carotid artery.
Carotid artery stents are made safe with the use of a filter that is parked above the plaque inside the artery and then removed after the case is finished to help catch any debris that might inadvertently be thrown off from the stent deploying.
Carotid artery stents can sometimes carry a high stroke risk depending on some factors including the aortic arch anatomy and also other features associated with the plaque itself. It’s best to discuss these options with your surgeon to better understand which option is best suited for you.
What is TCAR?
There is another alternative to carotid artery stenting through the groin artery that carries even lower risk of stroke and that is what is called a TCAR.
TCAR stands for Trans-Carotid Artery-Revascularization. This is when a small incision is made in the base of the neck above the collar bone and the CCA is used as the access point to insert the stent under the vision of X-ray. Another small puncture of the groin (femoral) vein is used to reverse the flow in the carotid artery during the deployment of the stent which prevents debris from traveling into the brain matter. This is a very fast procedure and the recovery period is short, with a low stroke rate making this a growingly more popular option.