Aneurysms
What is an Aneurysm?
An aneurysm is an abnormal enlargement or dilatation of an artery or part of an artery. An artery normally has a particular size and diameter. When the artery is larger than expected or has grown in a particular section to greater than the normal or expected size, it can be large enough to be called an aneurysm. An aneurysm is commonly defined as an artery that is at least 1.5 times greater than its expected, or ‘normal’ size.
How do they occur?
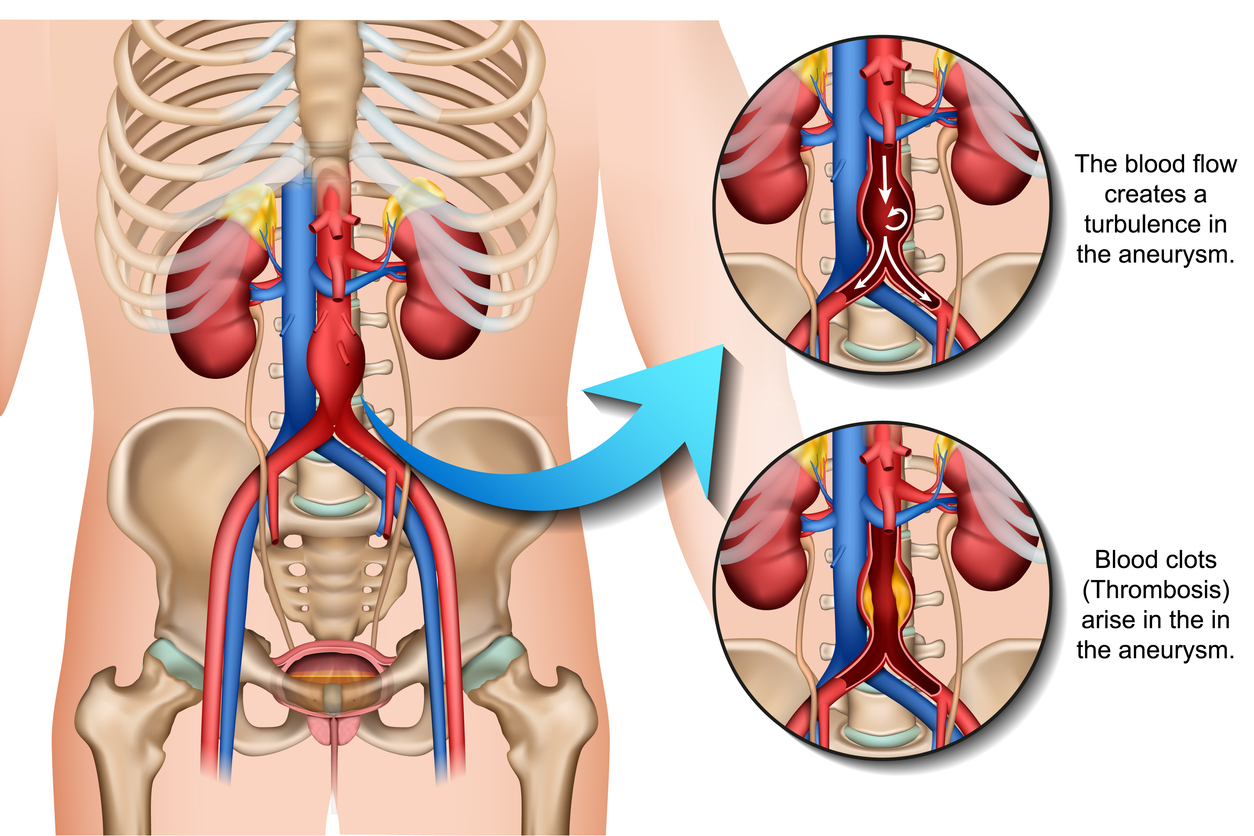
The normal arterial wall is designed to withstand the pulse of every heartbeat and at the same time adjust to the change in pressure. When the wall of the artery suffers from degeneration, weakness or damage then it can no longer withstand the normal changes in pressure and gradually dilates and stretches. This results in a ‘ballooning out’ of the artery.
What are the health factors that lead to Aneurysms?
- Smoking, Genetics, Blood Pressure, Sex, Age and Ethnicity can all play a role in Aneurysmal formation. Smoking is perhaps the most common cause and the most aggressive cause. Smoking causes degeneration (breaking down) of the arterial wall and ultimately aneurysmal dilatation.
- High blood pressure over a long period of time can sometimes cause aneurysmal dilatation or accelerate the growth of an existing aneurysm. High blood pressure can also cause a dissection to occur in the aorta which can then lead to an aneurysm.
- For reasons that are not fully understood, aneurysms that affect the Abdominal Aorta (AAA) are more common in males. As patients get older as well we know that aneurysms grow and get larger with time.
Why do I have an aneurysm?
- Depending on your risk factors, you may be more likely to have an aneurysm. Another factor that may make you more likely to have an aneurysm is having a sibling or parent with an aneurysm or having an aneurysm somewhere else in your own body.
- For example, a woman in her 40’s, who is found to have an abdominal aortic aneurysm (AAA), should tell their siblings or children in the future, to check for a AAA. Particularly if they themselves don’t have any other risk factors such as smoking.
- Another example is a man in his 70’s who has been smoking his whole life, who only has a small aneurysm, should let him brothers know that they should also be checked out for an aneurysm given the risk of a high genetic predisposition.
What should I be concerned about?
- Having an aneurysm may lead to harm and risk for you. It is always best to seek medical advice if you are unsure about any aspects of your health. If you have been found to have an aneurysm in any part of your body, it would be in your interest to see a specialist. There may not be anything to have done, but there may be a need to operate or intervene depending on many factors including the size of the aneurysm and the location in the body.
- Aneurysms that affect the Aorta in the Abdomen (AAA) are small when they are in between the diameter sizes of 3-4cm. When the AAA is between 4-5cm then this is something that should be watched closely. And when they are bigger than 5cm they should be potentially treated to prevent a rupture.
- A rupture is when the aneurysm is under significant pressure which leads to the aneurysm bleeding. This is a dangerous event that leads to internal bleeding. The mortality from a rupture is very high.
Should my family also be checked out?
- It’s always best to ask your specialist if any of your family members should be screened for an aneurysm. Often your siblings, children and parents (immediate family relations) could benefit.
- There may also be a benefit from screening other areas in your body for the potential presence of aneurysms. For example, a patient with a AAA may also have popliteal aneurysms (aneurysms in the leg behind the knee).
How are abdominal aortic aneurysms treated?
- Aneurysms can be treated with open surgical options and also endovascular or stenting options. For Many years prior to the technology of stenting, open repair was commonplace. It is still a good option for some patients today as it may offer a more durable option for those that require it.
- Open Surgical repair involves a 3-4 hours operation whereby the patient is put to sleep under a General Anaesthetic. The operation involves an incision through the abdomen. The aneurysm is then exposed through the abdominal cavity and then replaced with a tube. The synthetic tube is sewn onto the aorta above and below the aneurysm.
- Another option is Endovascular stenting, which avoids a large incision through the abdomen and allows a minimally invasive option to treat AAA’s.
- There are some other ways that an aneurysm can be managed which you should ask your specialist about.
What is an EVAR?
Endovascular Stenting of aneurysms have long been an interest as technology advances to reduce the need for open surgery on patients. Australia has been on the forefront of developing and leading the way in creating a good endovascular option for patients with AAA’s. EVAR, or Endovascular Aortic Repair, is now one of the main ways to treat AAA’s. It involves two small keyhole-like access points in the groin, both right and left. The stent grafts that are used to seal the aneurysm are inserted through the groin. The are inserted collapsed on a sheath which is deployed inside the aorta with the help of X-ray vision.
What is an Endoleak?
An endoleak is when there is still filling of the aneurysm sac despite an EVAR stent treatment. Sometimes, due to various anatomical or technical reasons, the sac can still be filled with blood which does not necessarily mean it is at risk of rupture. The most common Endoleak is what is called a Type 2 Endoleak. There are 4-5 different types of endoleaks that have well been described in the literature. Often you may read descriptions of endoleaks on scan reports. Its always best to speak with your specialist regarding any concerns you may have regarding an endoleak. Not all endoleak’s need to be treated, but of course there are some that are more concerning and may need treatment.
Why do I need to have repeat scans for the rest of my life?
Although EVAR is a good option and a non-invasive option for AAA treatment, with excellent recovery time, there is the need for long term surveillance. This surveillance comes in the form of repeat ultrasounds and sometimes CT scans. The reason for this is the sac of the aneurysm may evolve in time. The majority of AAA sac’s after EVAR shrink with time. This is the most desirable outcome. Some stay the same which as long as there are no concerns, may also indicate successful treatment with no need to be concerned. And then of course there are a smaller number that can unfortunately, despite an EVAR, still grow. This may be something that can be treated and fixed with another procedure.
Can I drive with an Aneurysm?
Driving with an aneurysm, in particular a AAA, may pose a threat to you and your passengers and also others driving or walking on the roads. As there is a rupture risk with most aneurysms, your safety and the safety of others need to be factored in when considering your driving ability.
Most of the time as long as you are under the management of a specialist, you can still drive. If your AAA is large, then treatment may be required in order for you to safely be driving. It is best to clarify these questions with your specialist.
