Peripheral Arterial Disease
What is Peripheral Arterial Disease (PAD)?
Peripheral Arterial Disease is a phrase used to describe arterial disease in the leg arteries but also the arteries arising from the aortic bifurcation. All these arteries are considered peripheral.
PAD occurs due to many causes but the most common is called atherosclerotic disease. Atherosclerotic disease develops for many reasons including smoking, high blood pressure, diabetes, high cholesterol and aging.
There are other more rare causes of PAD which include abnormal development of the arteries since birth, inflammation or infection of the vessels, autoimmune disease of the vessels and also repetitive injury to the vessels with time.
What is the anatomy of the arteries in the leg?
The aorta divides into iliac arteries. Both left and Right Iliac arteries then go on to supply the pelvis and the legs. The Iliac artery is then named the femoral artery in the groin and thigh. Then at the knee level it is known as the popliteal artery. Below the knee the popliteal artery divides into the anterior and posterior tibial arteries and the peroneal artery.
These arteries carry oxygenated blood from the heart to the feet and all the muscles and bones along the way. They are not to be mistaken with veins, which drain, or return, the deoxygenated blood from the feet and legs back to the heart.
What happens when the arteries get blocked?
When atherosclerotic disease develops, plaque starts to build up in the middle of the arteries. These arteries are sensitive to narrowing space as it needs to transport adequate blood to the organs, in this case the legs. When you walk and exercise, the muscles need more blood to function and use the oxygen the blood contains. If there is increased plaque and disease that narrows the centre of the vessels (the arteries) then there is a reduction in the volume of blood delivered. Therefore the muscles in the legs and feet can cramp and become tired. This is commonly referred to as claudication.
Sometimes the Plaque can be so severe that the entire segment or section of the artery can be blocked with a complete occlusion. This can be quite serious and can cause severe symptoms. When there are multiple blockages in the same leg then the symptoms can progress from not just developing pain when exercising but pain all the time. Even when at rest or sleeping. This is quite a serious level of disease and indicates that the muscle, skin and tissue is at risk of potentially dying.
In the more advanced levels of disease, patients could develop gangrene. Gangrene is a severe degree of PAD. It indicates that the vessels are so blocked that tissue has no more oxygen to survive as the arteries are unable to supply it.
Can my arteries return to normal?
It is a very difficult and unlikely process to reverse plaque naturally or without intervention. But there are medications and strategies to help reduce the progression and even halt the development of further plaque.
Medications such as Statins, or cholesterol lowering medications (Rosuvastatin, Simvastatin, Ezetimibe, Atorvastatin) can help stabilize and reduce the progression of plaque. Your doctor may also prescribe a low dose of daily aspirin for you as it has been shown to reduce the risk of what’s called a ‘cardiovascular event’ when patients have PAD. A Cardiovascular event is either a stroke or a heart attack.
What if I need my arteries unblocked?
Unblocking arteries are what vascular surgeons are trained to do from the earliest steps of their career. They are trained in both surgical and endovascular or minimally invasive techniques to unblock arteries.
Dr Nedal Katib has a deep interest in treating lower limb arterial disease with endovascular minimally invasive techniques. These techniques utilise Xray and contrast dye to visualise the artery and the blocked that are needed to be treated without surgery. Using wires, catheters, balloons and stents, Dr Katib treats such blockages without having to perform open surgery.
There are many strategies that can be taken to unblock arteries. There is also a strategy on weighing up the risks and benefits of treating each individual blockage and bringing together the safest and most likely successful plan for your type of disease and current state. Achieving success in this area is not always straightforward and each patient may require a different strategy. It’s best to understand and discuss these strategies with Dr Nedal Katib.
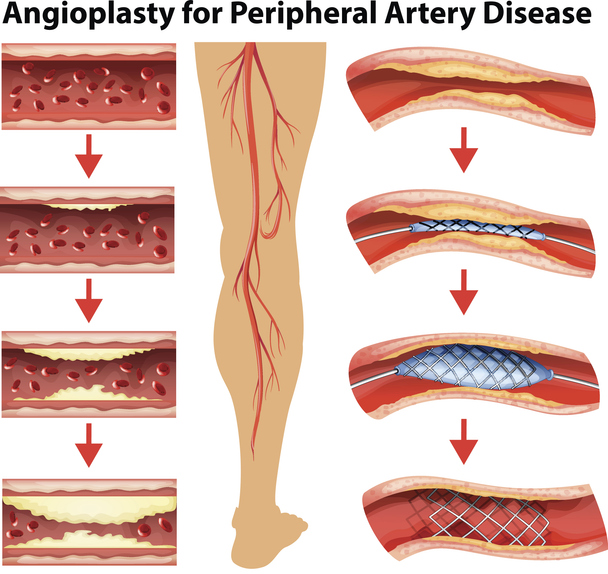
What is involved with an Angiogram and Angioplasty?
An Angiogram is when, through a small catheter placed in the artery through a small hole in the skin, contrast dye is injected into the bloodstream and with Xray vision the artery is lit up and the blockages are made clear. This then gives Dr Katib a roadmap to identify where and what he needs to treat.
What is a stent?
A stent is a scaffold that holds the artery open allowing the blood to flow through without hindrance. Stents are usually made of some form of metal. Stents typically used in Dr Katibs Practice are either Bare Metal or Nitinol. Nitinol is made of Nickel and Titanium. These are robust and allow for a long lasting effect in your arteries. They are inert and mostly can be used with MRI imaging. They very rarely cause any reaction in your body and very rarely get infected.
Some stents can be ‘covered’ which is when a stent is covered with a plastic lining. This extra layer sometimes is necessary to prevent blood getting around the stent or from disease building up inside the stent. Covered stents are not as commonly used for blocked arteries but are more commonly used for bleeding vessels or for aneurysms.
What is a Bypass?
When a segment of blocked artery can’t be treated with a stent or a balloon, then a bypass is when another tube is sewn on to the artery above and below the blockage, allowing for the blood to bypass the blocked segment.
The newly sewn on tube can either be your own vein (remember veins are different to arteries, the veins drain blood from the foot to the heart, but there are a lot of veins that can be taken out of your leg without harming the leg or affecting its drainage) or it can be a plastic tube thats sterilised and made especially for bypasses.
Bypass operations involve a long procedure that can take several hours and involves at least two incisions through the leg. The recovery time is variable but ranges between 4 days to 4 weeks. This depends largely on the initial symptoms and also how complex the operation becomes. There are also many other factors relating to the patient’s overall health that determines the recovery time.
Bypass operations are considered ‘open’ operations and have always been the traditional way in dealing with blocked arteries prior to the introduction of endovascular surgery or minimally invasive surgery.
Is my leg at risk of being amputated?
Vascular disease, Diabetes and Renal Failure are all conditions that can have variable severity and result in differing outcomes. Advanced disease in a patient’s arteries can result in severe and irreversible damage to the leg and may result in amputation of the leg if left untreated.
Amputation of the lower limb is a debilitating and very morbid procedure. It can lead to a serious decline in overall health and function.
Dr Nedal Katib strives hard and is passionate about Limb Salvage. Which is preventing the outcome of amputation by improving blood supply to the leg, eradicating infection and healing long standing wounds and ulcers.
